Researchers Identify Potential Target for Treating Primary Sjogren’s Syndrome
Lower levels of Gαq — a protein that regulates many aspects of immune responses — appear to drive the progression of primary Sjogren’s syndrome by increasing a subset of pro-inflammatory immune cells, a study shows.
The study, “Expression of Gαq Is Decreased in Lymphocytes from Primary Sjogren’s Syndrome Patients and Related to Increased IL-17A Expression,” was published in the Journal of Immunology Research.
Sjogren’s syndrome is an autoimmune disease where the immune system incorrectly recognizes secretory glands as foreign and attacks them. The lacrimal and salivary glands are the most affected in these patients, resulting in dry eyes and dry mouth.
Because little is known about the disease, patients are often diagnosed at late stages, when the glands have been irreversibly damaged and effective treatments are limited. Researchers are working to better understand the disease and identify targets for its early diagnosis and treatment.
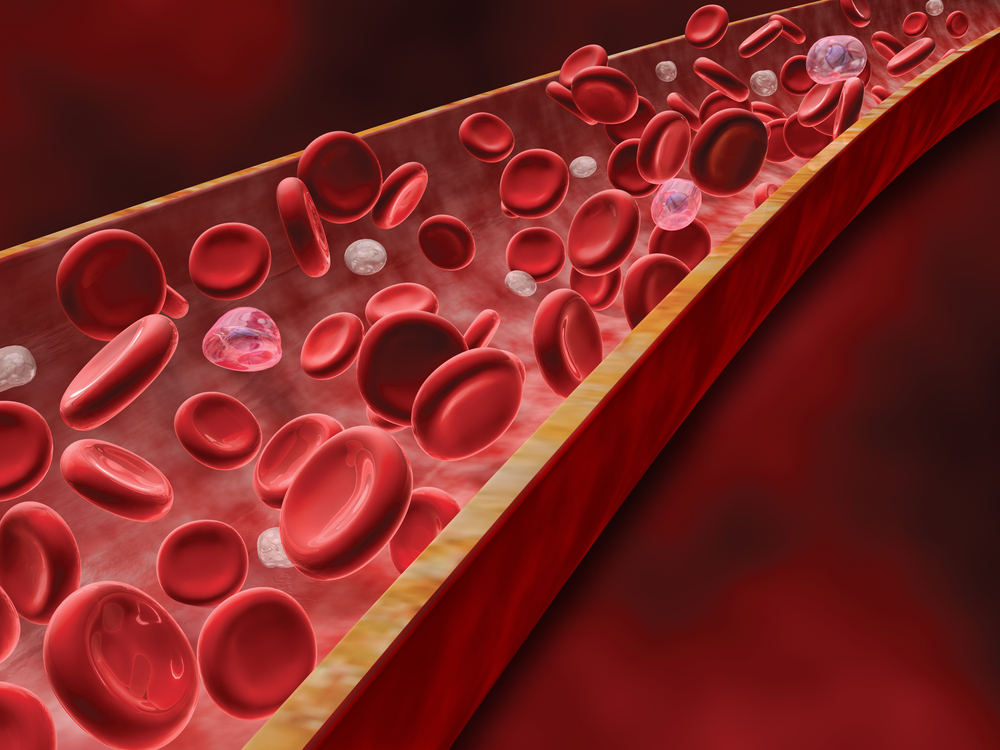
A group of immune cells, called T helper type 17 (Th17), have been identified as the key cells driving inflammation and autoimmunity. In primary Sjogren’s syndrome, Th17 cells are increased and drive the damage of glands. But how they are regulated in these patients is still unknown.
Previous research identified a subunit of the Gq protein, called Gαq, as a player in rheumatic diseases like lupus and rheumatoid arthritis. These conditions are also linked to Th17 activity, suggesting that Gαq may affect these cells and impact disease activity.
In an attempt to address this question, researchers examined the role of Gαq in patients with primary Sjogren’s syndrome. They enrolled 39 patients and 40 healthy controls and compared the levels of Gαq in blood cells with other clinical characteristics.
Gαq levels were significantly lower in patients with Sjogren’s syndrome compared to those of healthy controls. And the lower the levels, the more severe the disease, supporting a role for Gαq in Sjogren’s syndrome.
Researchers suspected that Gαq worked to block the differentiation of Th17, and that patients with lower Gαq would have more of these immune cells and increased disease severity. To test this, they examined the levels of an inflammatory molecule called IL-17A that is produced by Th17 cells.
As expected, Sjogren’s patients had higher levels of the pro-inflammatory molecule. They also found that Gαq levels were inversely correlated with IL-17A levels, “revealing a novel regulation mechanism for the abnormal Th17 levels in patients with pSS [primary Sjogren’s syndrome],” investigators wrote.
“These results provide a new mechanism for [primary Sjogren’s syndrome] pathogenesis regarding abnormal Th17 cell regulation,” researchers concluded.