Sjögren’s Patients Have Higher Risk for Aortic Complications, Study Finds
Written by |
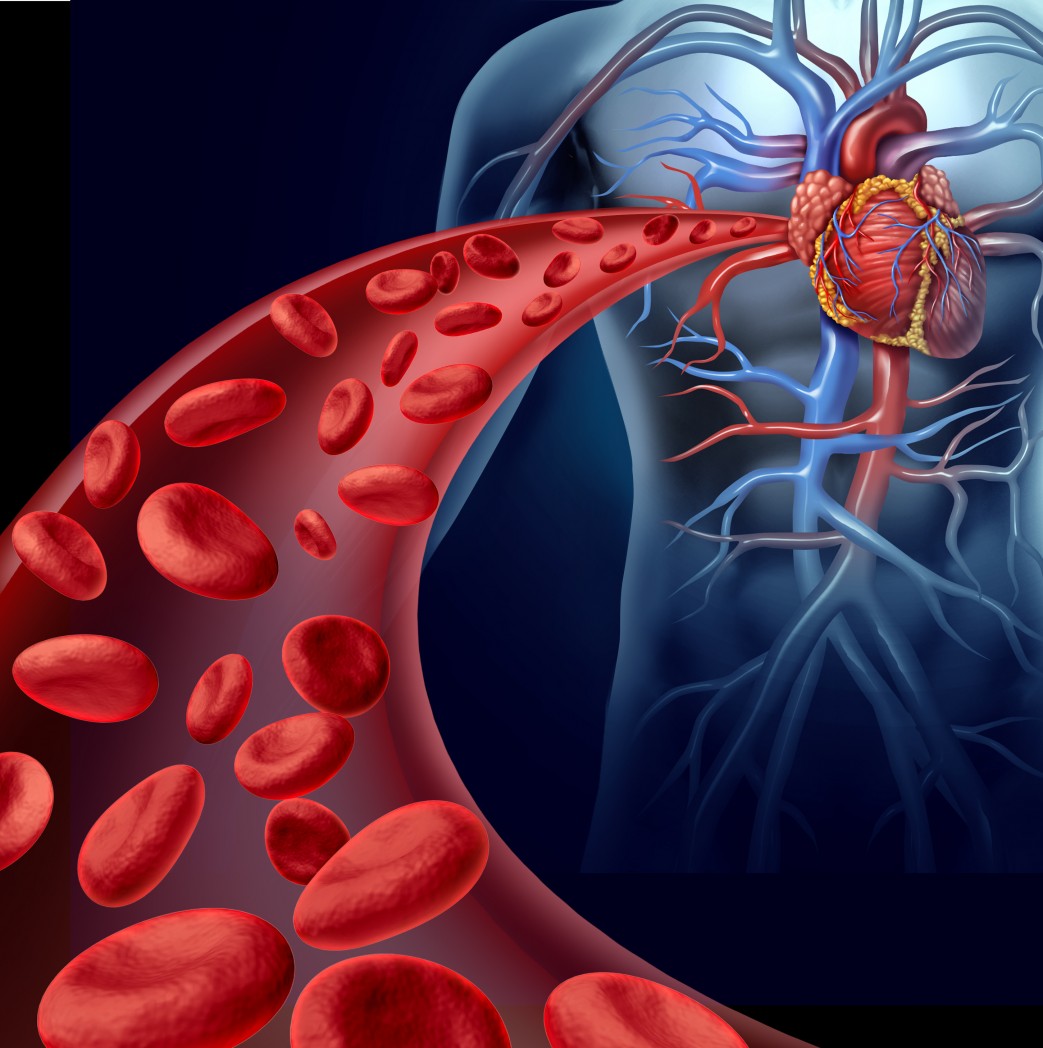
Sjögren’s syndrome patients are more likely to experience both aortic aneurysms and aortic dissection — two medical complications that affect the wall of the aorta, the largest blood vessel in the body that carries blood from the heart to the rest of the body.
The study with that finding, “Increased risk of aortic aneurysm and dissection in patients with Sjögren’s syndrome: a nationwide population-based cohort study in Taiwan,” was published in BMJ Open.
Sjögren’s syndrome is a chronic autoimmune disease characterized by an abnormal infiltration and accumulation of immune cells inside certain glands, leading to tissue inflammation and eventually irreparable damage. As a result, patients affected by the condition usually experience extreme dryness in the eyes and mouth.
Aortic aneurysms (AAs) occur when an abnormal bulge appears in the wall of the aorta, compromising blood flow from the heart to the rest of the body. AAs increase the risks of aortic dissection (AD), a serious condition in which the inner layer of the aorta tears and blood rushes through the tear, separating (dissecting) the inner and middle layers of the vessel. Both AAs and ADs usually are fatal.
Previous studies already demonstrated that AAs are more prevalent in patients with autoimmune diseases, including rheumatoid arthritis and systemic lupus erythematosus, compared with the general population. In addition, several molecular mechanisms that have been implicated in Sjögren’s, also participate in the onset and progression of AA and AD, suggesting that the condition could be linked to these aortic complications.
In this retrospective study, researchers set out to investigate whether Sjögren’s patients have higher risk for AA or AD.
Clinical data from 10,941 patients and 43,764 control subjects were extracted from Taiwan’s National Health Insurance Research Database (NHIRD) between 2000 and 2010.
After a follow-up period of 10 years, Sjögren’s patients had significantly higher prevalence of AA or AD compared to controls (0.43% vs. 0.37%). Interestingly, the incidence for AA or AD was higher in males and older patients, regardless of whether these patients suffered from Sjögren’s.
Additional analysis revealed that Sjögren’s patients — regardless of being diagnosed with the primary (unknown cause) or secondary (associated with other medical conditions) form of the disease — had a significantly higher risk of developing both AA and AD compared to control subjects.
Together these findings strongly suggest that Sjögren’s patients have higher risks of developing AA or AD. Authors also stressed the importance of increased surveillance and risk awareness by physicians treating patients with Sjögren’s syndrome.
“Healthcare professionals should be aware of these life-threatening aortic events and aim to make early diagnosis of AA or AD. When patients with [Sjögren’s syndrome] present with chest, back or abdominal symptoms, the possibility of AA or AD should be considered, with a specific and rapid examination,” researchers wrote.
“Although our study identified the association between [Sjögren’s syndrome] and AA/AD, the cohort study design did not enable determination of the cause-effect relationship. Further prospective follow-up studies, mechanistic studies and animal experiments should be performed,” they added.





