Rheumatoid Factor Subtype Can Serve as Diagnostic Marker for Primary Sjogren’s, Study Says
Written by |
A subtype of rheumatoid factor targeting a class of antibody called immunoglobulin A can be used as a diagnostic and predictive marker for primary Sjogren’s syndrome, a new study shows.
The study, “Clinical and diagnostic significance of serum immunoglobulin A rheumatoid factor in primary Sjogren’s syndrome,” was published in the journal Clinical Oral Investigations.
Primary Sjogren’s syndrome (pSS) is a chronic autoimmune disease where the immune system attacks secretary glands, including the glands producing tears and saliva. This leads to dryness in the main mucosal surfaces such as the mouth, eyes, nose, pharynx, larynx, and vagina.
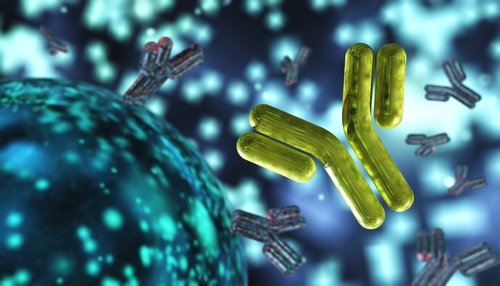
Autoantibodies, or antibodies against the body’s own tissue, are the major cause of the disease. Among them lies a class of antibody called rheumatoid factor (RF), which target a patient’s own antibodies.
Essentially, RF is an antibody against an antibody. Rheumatoid factors can be directed toward different immunoglobulins, or antibodies, which include IgA, IgG, and IgM. Each immunoglobulin is different in their structure, targets, and function.
Between 75-95% of pSS patients are positive for rheumatoid factor, which has been shown to be correlated with prognosis and renal involvement.
Specifically, IgA-targeting RF has been most commonly reported, with a prevalence ranging from 25.8% to 86% of pSS patients.
Clinically, pSS is difficult to diagnose due to a lack of a single diagnostic test. There are various classification criteria that have been designed for clinical trials and research, but are often used to make a diagnosis in individual patients with suspected primary Sjogren’s syndrome.
“We have encountered a few patients who failed to meet the classification criteria, but have had clinical features highly suggestive of a diagnosis of pSS,” researchers wrote.
So they conducted a study to determine if any particular type of rheumatoid factor (IgA, IgG, or IgM) carries a potential diagnostic value for detecting primary Sjogren’s.
Additionally, researchers assessed whether IgA RF levels could serve as a predictive factor by analyzing their association with clinical characteristics.
Researchers measured rheumatoid factor levels in 77 patients with pSS and 37 patients with idiopathic sicca symptoms.
Sicca syndrome refers to a disease characterized by dryness of mucosal surfaces, especially in the eyes and mouth, similar to pSS but without any evidence of autoimmune disease.
Researchers found that IgA and IgG rheumatoid factor levels, but not IgM, were significantly higher in patients with pSS, compared to the idiopathic sicca symptom group.
Additionally, testing for IgA rheumatoid factor demonstrated 83.1% sensitivity (true positive rate) and 78.4% specificity (true negative rate) in the diagnosis of pSS.
Analyzing IgA RF levels in relation to clinical characteristics showed that IgA rheumatoid factor levels correlated with levels of antinuclear antibodies, high IgG and IgM levels, and low C3 levels in patients. All these factors are characteristic of an active autoimmune disease.
Results also showed that IgA RF levels were associated with dry mouth, severe sialo scintigraphic grade, and low unstimulated salivary flow rate, which are factors indicative of worse salivary gland function.
“Our findings confirmed the potential of IgA RF to distinguish pSS from idiopathic sicca symptoms,” researchers wrote.
“We suggest IgA RF as an additional clinical predictive and diagnostic marker for pSS,” they added.