Primary Sjogren’s Patients Have Altered Levels, Activity of Immune Cells, Study Finds
Patients with primary Sjogren’s syndrome (pSS) show altered levels of specific types of immune T-cells and B-cells, which may play an important role in disease activity, new research from Norway suggests.
The study, “T follicular-like helper cells in the peripheral blood of patients with primary Sjogren’s syndrome,” was published in the Scandinavian Journal of Immunology.
The infiltration of salivary and lacrimal glands by white blood cells cause dry eyes and dry mouth in primary Sjogren’s patients, as well as other symptoms, such as inflammation and fatigue.
B-cells are a type of white blood cell that are key to the development of pSS. In turn, T follicular helper (TFH) cells — found in secondary organs of the immune system, including the spleen and lymph nodes — are crucial for the survival, development, and function of B-cells.
TFH cells act on B-cells through molecules such as CXCR5, ICOS and PD-1, while also playing an important role in the response of immune cells against pathogens.
The scientists assessed TFH cells and explored their potential relationship with B-cell subtypes, namely memory B-cells, formed after a primary infection and important for robust responses to re-infections; plasma cells, immune cells that produce a single kind of antibody; and plasmablasts, or immature plasma cells, in the blood of primary Sjogren’s patients.
The investigators also evaluated the correlation of the TFH-B-cell relationship with clinical findings in patients with pSS and levels of Ro/SSA and La/SSB autoantibodies, which are characteristic in these patients.
A total of 32 subjects — 16 pSS patients with a mean age of 60 and 16 controls with a mean age of 52 — were included in the study. Both groups had 13 women and three men.
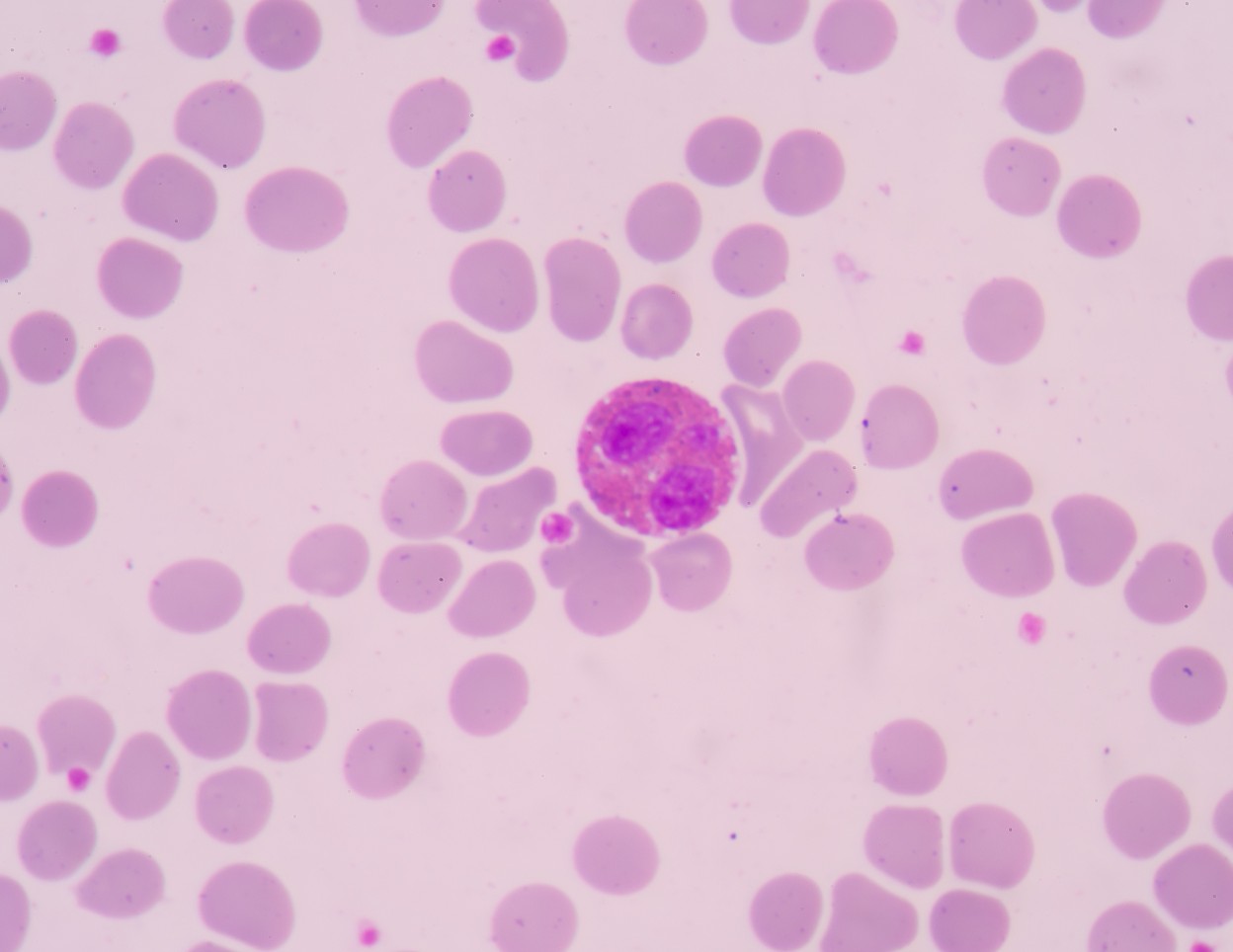
The scientists defined four subsets of TFH-like cells containing the T-cell protein markers CD3, CD4, and CXCR5, which mediates the migration of T-cells and B-cells. These specific TFH cell subpopulations varied as to whether or not they expressed ICOS and PD-1.
Compared to controls, pSS patients showed higher fractions of plasmablasts and THF immune cells containing both ICOS and PD-1, or containing ICOS but not PD-1.
But two subtypes of memory B-cells, which differed in activity of the CD38 marker, were lower in patients with pSS, which “may indicate previous activation and differentiation into antibody-secreting cells,” the scientists wrote.
The data also revealed that in primary Sjogren’s patients, but not in controls, the higher the number of TFH cells, the higher the levels of plasmablasts and plasma cells, which matches previous reports, the authors noted.
Results also showed a correlation between autoantibody levels and increased TFH immune cells, plasmablasts and plasma cells, as well as reduced numbers of memory B-cells. In pSS patients, memory B-cells not expressing CD38 showed a higher response to stimulation with Ro/La proteins, compared to controls.
Also, the investigators found that disease activity in primary Sjogren’s syndrome patients induced a trend toward higher TFH cells and lower B-cell numbers, as well as increased activation of B-cells.
“Overall, we believe our findings indicate an association between the TFH-like cells and B cell activity in pSS, which may be an implication in the disease development, but further studies have to be carried out to elucidate this,” the researchers wrote.