Ly9 Activation Reduced Potential Damage to Salivary Glands and Kidneys in Mouse Model of Sjögren’s Syndrome
Written by |
Activating the immune receptor Ly9 significantly reduces the infiltration of immune cells into the salivary glands and kidneys of mice with Sjögren’s syndrome-like disease, without compromising their general immune system — making it a potential therapeutic target for the chronic condition, a study finds.
The study, “Ly9 (CD229) Antibody Targeting Depletes Marginal Zone and Germinal Center B Cells in Lymphoid Tissues and Reduces Salivary Gland Inflammation in a Mouse Model of Sjögren’s Syndrome,” was published in Frontiers in Immunology.
Sjögren’s syndrome is a chronic condition affecting mostly women, where immune cells infiltrate and damage certain glands in the body, such as those producing tears and saliva. A hallmark of the disease is dryness of the eyes and mouth, but patients often present other systemic symptoms, including pneumonia, kidney disease, and B-cell lymphomas.
Sjögren’s patients have excess amounts of a kind of B-cells called marginal zone B-cells (MZB cells), which are critical players in the condition, and are the main cause of lymphomas in these patients.
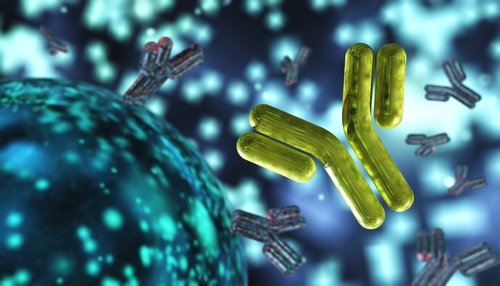
Researchers have found that the Ly9 cell surface receptor, found in virtually all B- and T-cells — with particularly higher levels in MZB cells — is important for keeping the immune system in check. Activating this protein reduces B-cell responses and selectively eliminates MZB cells in the spleen, where they are normally found.
Thus, the scientists explored the therapeutic potential of Ly9 activation in a mouse model with autoimmunity that mimicked the features of Sjögren’s syndrome. At 24 weeks, these female mice showed signs of immune cell infiltration in their salivary glands and kidney inflammation, and had autoantibodies in circulation, such as anti-Ro and anti-dsDNA.
As expected, treatment with an anti-Ly9 activating antibody at 24 weeks significantly reduced the amount of MZB cells in the spleen. But researchers found that other subsets of spleen B-cells involved in Sjögren’s development — B1 and germinal center (GC) B-cells — were also reduced after treatment.
Ly9 targeting also lowered the amount of MZB cells and immune aggregates in salivary glands and lymph nodes in the mice, compared with those given the placebo treatment. This happened, in part, because the immune cells lost some adhesion molecules that help them enter these tissues, the researchers found.
After seeing the benefits of this approach, the team hypothesized that Ly9 treatment could prevent symptoms from appearing in younger, 12-week-old mice. While placebo-treated animals started showing signs of immune infiltration in salivary glands after two weeks, mice treated with a single injection of the antibody showed no signs of immune cell accumulation.
Researchers also found that the treatment lowered kidney inflammation, and reduced the amount of some autoantibodies in circulation. Interestingly, the antibody did not cause a generalized suppression of the immune system, which is often a concern with medications targeting immune function.
“Our results show that Ly9 antibody targeting selectively depletes MZ, B1 and germinal center (GC) B cells in lymphoid tissues, and decreases lymphocyte infiltration in the salivary glands and kidney by modulating B cell activation and trafficking of T and B cells to inflammation sites,” the scientists wrote.
“The results of this study demonstrate that antibody targeting of the cell surface molecule Ly9 (CD229) can restrain spontaneous autoimmune disease in a mouse model of SjS (Sjögren’s syndrome),” they concluded.