Survey: Sjögren’s Patients Satisfied With Care, Pessimistic About Future
Written by |

Note: This story was updated Dec. 21, 2021, to note that Sjögren’s syndrome is not a rare disease, being estimated to affect 1-4 million people in the United States.
While the vast majority of people with Sjögren’s syndrome are satisfied with their healthcare provider and medication, more than one in three are dissatisfied with their overall quality of life, and a similar number report being pessimistic about the future, according to a U.S.-based survey conducted by Sjogren’s Syndrome News.
Conducted from May 11 to Aug. 18, the online survey sought to gain greater understanding of the Sjogren’s community, focusing on disease management, treatment plans, medication side effects, insurance, and patient quality of life. It was conducted in collaboration with Bionews Insights, the research arm of Bionews Services, which publishes the Sjogren’s Syndrome News website.
“As we see with many diseases, there are significant populations of Sjogren’s syndrome patients who are unsatisfied with their quality of life and/or pessimistic about their futures. These are understandable feelings in response to the circumstances and, yet, also point out the need for further resource allocation to the understanding and improvement of these outcomes,” Jacob Harney, PhD, the research lead at Bionews Insights, said in a statement to Sjogren’s Syndrome News.
“Bionews insights is presently conducting research into quality of life indicators across many disease communities. It is our mission to always be working toward improving patient outcomes for all our communities,” Harney added.
Who answered the survey?
A total of 743 people completed the survey, most of whom — 725, or 97.58% — were patients living with Sjögren’s. The remaining respondents were mostly family members or caregivers of someone with the disease.
The subsequent analysis focused on patients only, the majority of whom (701 of 724 respondents, 96.82%) identified as female. The average age was 61.9 years, based on 493 responses, and the average time spent living with Sjögren’s was just more than five years, according to 443 responses.
Of 721 respondents who specified their race, the majority (91.54%) were white. Additionally, 2.36% identified as Black/African American and 2.77% as mixed race. Other races each accounted for fewer than 1% of respondents.
Most patients who responded to a question about education (721) held either a bachelor’s degree (29.27%) or a graduate degree (28.43%; master’s, doctorate, law, or medical degree). Another 26.49% had completed an associate’s or trade school degree, while 15.81% had a high school diploma or GED.
Among the 536 patients who reported their annual income, 24.25% made less than $30,000 per year, 22.58% had an income of $30,000–$60,000, 30.04% of $60,000–$100,000, and 23.13% of more than $100,000.
Of the 720 patients who reported their type of Sjögren’s, more than half (58.19%) had primary disease and 11.11% had secondary disease; the remaining respondents said they didn’t know their disease type. There were 101 patients who reported having a biological relative with Sjögren’s, based on 719 responses.
The most common Sjögren’s symptoms — affecting more than half of the 721 patients who responded to this question — were dry eyes (93.75%), dry mouth (93.06%), joint pain, swelling, or stiffness (80.02%), prolonged fatigue (72.12%), and prolonged dry skin (67.54%). Symptoms with the most profound effect on daily activities, based on 715 responses, were prolonged fatigue, dry eyes, dry mouth, and joint pain, swelling, or stiffness.
In addition to Sjögren’s syndrome, 145 of 697 patients had rheumatoid arthritis, 62 had lupus, 15 had scleroderma, and one had multiple sclerosis.
When asked about health insurance, the majority of patients reported having Medicare (49.79%) or private insurance (42.02%). Only two of the 721 patients who reported their insurance said they had none.
How were the patients being cared for?
The most common types of doctors seen to manage Sjögren’s, based on 721 respondents, included a rheumatologist (85.02%), a primary care doctor (59.22%), and an ophthalmologist (44.38%).
More than two-thirds (71.03%) of patients were taking medications to treat Sjögren’s syndrome, based on 718 responses. In addition, 667 of 721 patients (92.51%) also were taking medications unrelated to Sjogren’s.
The most commonly used treatments for Sjögren’s, based on responses from 721 patients, were Plaquenil (hydroxychloroquine), used by 42.70%, and Restasis (cyclosporine ophthalmic emulsion), used by 18.44%.
From 510 responses, the most frequently reported treatment side effects were itchy or irritated eyes (52.74%), fatigue (50.98%), and joint pain (45.09%). Fatigue frequently was specified as the most bothersome side effect, but abdominal pain was the side effect that made most patients consider a change in medication.
The majority of patients (61.67%, or 444 of 720) said that they previously had not been on treatments for Sjögren’s that they since had stopped taking. For those who had discontinued a treatment previously, the therapies stopped most often were Plaquenil and Salagen (pilocarpine), and the most common reason for stopping those meds was side effects.
Two patients reported having undergone an organ transplant related to Sjögren’s. One had received a lung transplant, and the other had received both a liver and kidney transplant.
How did patients feel about their quality of life and care?
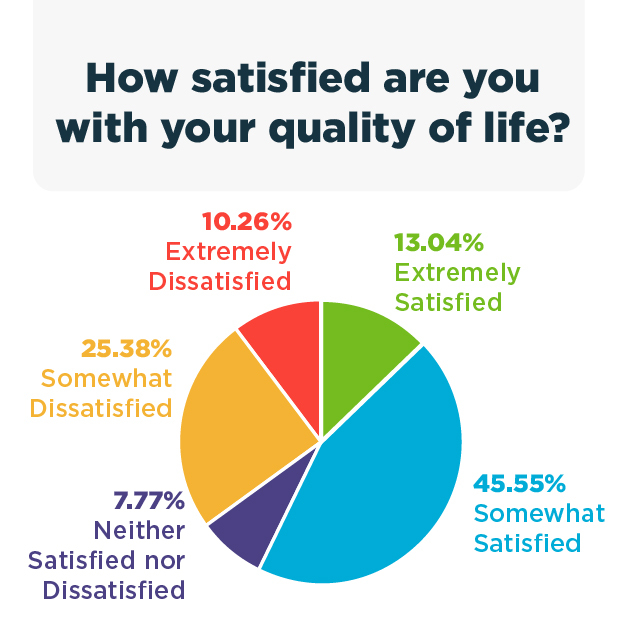 Among the 721 patients who answered a question about their quality of life, 13.04% were “extremely satisfied” and 43.55% “somewhat satisfied.” However, more than a third of patients said they were dissatisfied with their life quality: 25.38% were “somewhat dissatisfied,” and 10.26% were “very dissatisfied.”
Among the 721 patients who answered a question about their quality of life, 13.04% were “extremely satisfied” and 43.55% “somewhat satisfied.” However, more than a third of patients said they were dissatisfied with their life quality: 25.38% were “somewhat dissatisfied,” and 10.26% were “very dissatisfied.”
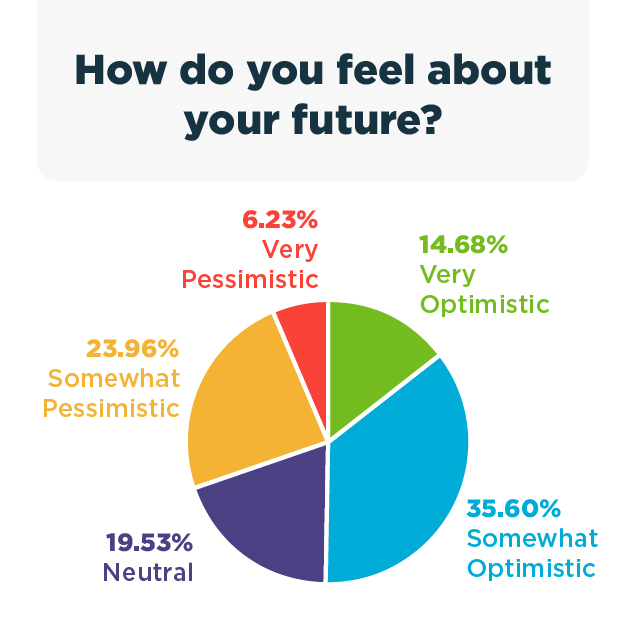
Similarly, based on 722 responses, 14.68% of patients were “very optimistic” about the future and 35.60% were “somewhat optimistic.” However, just less than one-third were pessimistic about the future: 23.96% were “somewhat pessimistic” and 6.23% were “very pessimistic.”
Patients generally were satisfied with their medications and healthcare. Of the 719 patients who rated their satisfaction with their healthcare providers, 41.17% were “extremely satisfied” and 36.58% were “somewhat satisfied,” while 7.93% said they were “somewhat unsatisfied” and 2.5% “extremely dissatisfied.”
Overall, a slim majority of patients were satisfied with their current treatment, though exact rates varied based on the specific medication. For example, of 274 who reported their satisfaction with the most commonly used treatment, Plaquenil, 24.09% were “extremely satisfied” and 44.89% were “somewhat satisfied,” whereas 9.12% were “somewhat dissatisfied” and 1.82% were “very dissatisfied.”
For the next most common medicine, Restasis, 23.39% of the 124 patients who reported their satisfaction were “very satisfied” and 51.61% “somewhat satisfied,” while 10.48% were “somewhat dissatisfied” and 1.61% “very dissatisfied.”
In line with the high satisfaction rates for treatments, few patients said they were thinking about changing therapies. For all of the most commonly used medications, less than 15% of respondents indicated they were considering switching therapies. Among the 122 patients who were considering switching, the main reasons were effectiveness (44.26%) and side effects (26.23%).
Of note, most patients said they were likely to participate in clinical trials, with 26.91% “extremely likely” and 34.81% “somewhat likely,” based on 721 responses. Also, based on 717 responses, 76.85% of patients expressed interest in learning more about clinical trial opportunities.
Overall, the survey results highlight generally high rates of satisfaction with care. Nonetheless, “there is still significant need for the development of further treatments for the Sjögren’s community,” Harney said.
“Development of medications/therapies that can address the most common symptoms more effectively (dry eyes and mouth, joint pain, swelling, stiffness, prolonged fatigue, and prolonged dry skin) than present options could help address quality of life significantly,” he added.