Sjögren’s Syndrome Patients Have High Risk of Cardiovascular Disease, Study Suggests
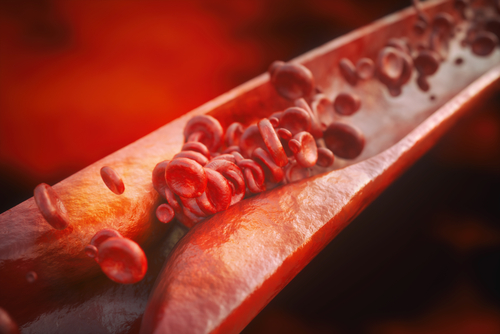
Patients with primary Sjögren’s syndrome (PSS) have stiffer arteries and more atherosclerotic plaques than control subjects without the disease, a study found. The findings suggest that PSS patients have a higher risk of cardiovascular diseases.
The study, “Association between primary Sjogren’s syndrome, arterial stiffness, and subclinical atherosclerosis: a systematic review and meta-analysis,” was published in Clinical Rheumatology.
Sjögren’s syndrome is a chronic autoimmune disease characterized by abnormal infiltration and accumulation of immune cells inside some glands, leading to tissue inflammation and eventually irreparable damage.
The disorder is considered primary when there is no underlying cause, or secondary when it occurs with other autoimmune diseases, such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
In RA and SLE, patients experience acute systemic inflammation accompanied by chronic vasculitis, or inflammation of the blood vessels’ walls. This leads to the formation of atherosclerotic plaques. Ultimately, these conditions may cause cardiovascular disease, one of the main causes of death among these patients.
This systematic review focused on exploring the relationship between arterial stiffness — an alteration of blood vessels that can occur as a result of vasculitis — and subclinical atherosclerosis (early asymptomatic atherosclerosis) in the context of PSS.
Eight observational studies involving 767 participants were included in the meta-analysis. Two of these studies used pulse wave velocity to assess arterial stiffness, and five used intima-media thickness to determine structural alterations in blood vessel walls that usually occur in subclinical atherosclerosis. One additional study measured both parameters.
Pooled results from all of the studies revealed a significant increase in both measures in PSS patients compared to control subjects. This suggests that PSS is directly associated with arterial stiffness and subclinical atherosclerosis.
“Our study suggests that PSS is associated with arterial stiffness and subclinical atherosclerosis. More large-scale studies need to be conducted to find the correlation of subclinical atherosclerosis in PSS with the cardiovascular or cerebrovascular event,” and to determine how PSS leads to increased arterial stiffness, researchers wrote.
“Randomized controlled trials or prospective cohort studies to explore the benefit of statins, controlling cardiovascular risk factors or disease activity could potentially help providers in improving patients’ general health and avoiding progression of atherosclerosis, ” they added.






