Tooth Stem Cell Secretions May Help Treat Sjögren’s
Written by |
Signaling molecules secreted by stem cells in teeth have anti-inflammatory properties that could be useful for the treatment of Sjögren’s syndrome, recent research in mice shows.
The findings were published in Stem Cell Research & Therapy, in the study, “Secreted factors from dental pulp stem cells improve Sjögren’s syndrome via regulatory T cell-mediated immunosuppression.”
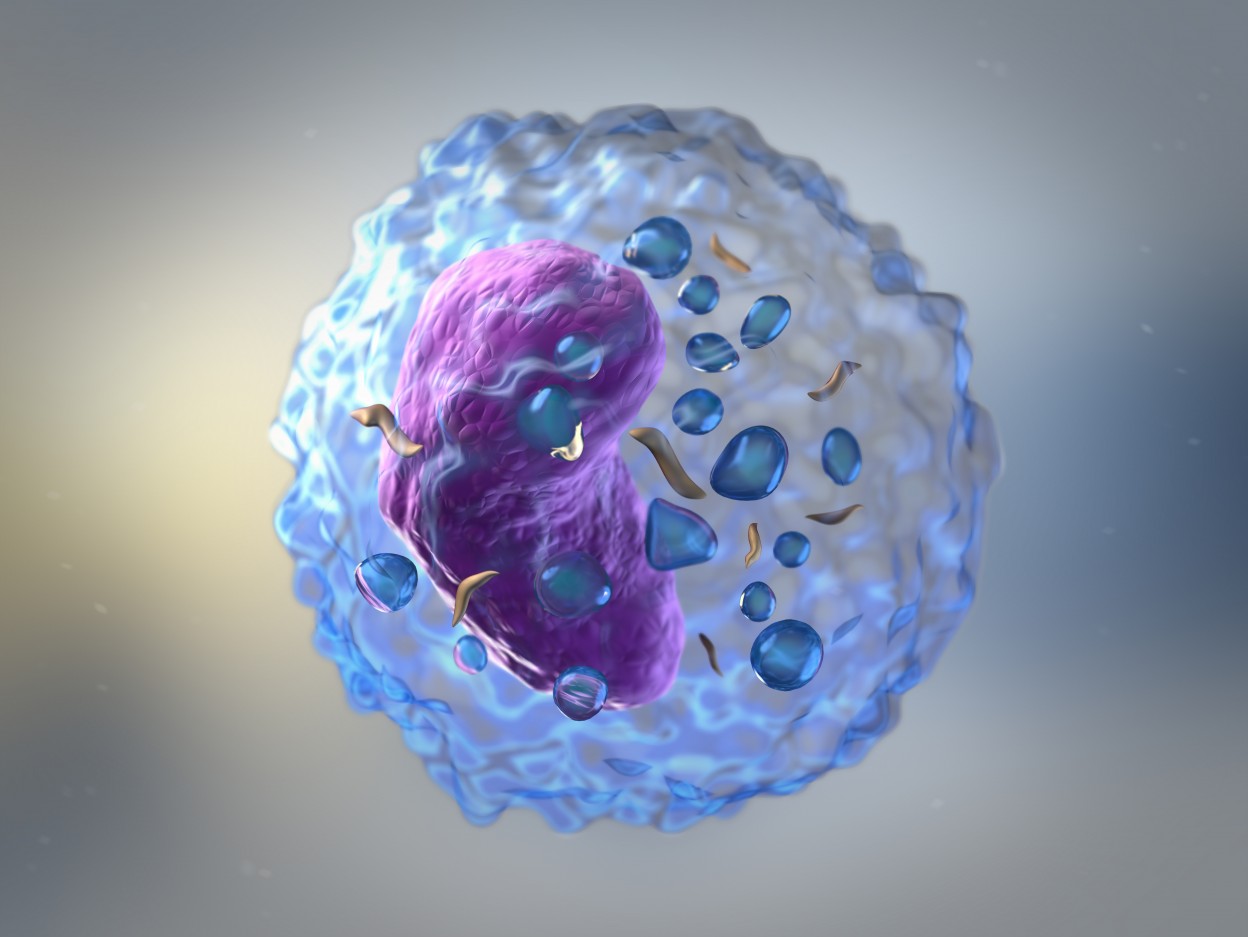
Stem cells are able to grow and differentiate into other kinds of cells. There are several different kinds of stem cells with different biological functions in the body. Stem cells often secrete signaling molecules to communicate with the cells around them and these signaling molecules often have anti-inflammatory properties.
In the new study, researchers at Kyushu University, in Japan, tested the anti-inflammatory effects of substances secreted by two types of cells: dental pulp stem cells (DPSCs), which are stem cells found in the soft living tissue in teeth, and bone marrow mesenchymal stem cells (BMMSCs), which are found in bone marrow.
The researchers grew the respective cell type in a culture, then analyzed the molecules secreted by the cells into the surrounding liquid. Dozens of signaling molecules were assessed; broadly, the researchers noted that DPSCs secreted more anti-inflammatory molecules than BMMSCs.
Sjögren’s syndrome is caused by the immune system attacking the body’s tear and saliva glands, leading to dryness in the eyes and mouth. This immune attack is driven largely by a type of immune cell called T-cells.
The researchers found that exposure to signaling molecules from DPSCs decreased the number of T-cells expressing pro-inflammatory markers, and to a greater degree than exposure to molecules from BMMSCs.
In these experiments, the researchers treated T-cells with media that had been “conditioned” by DPSCs or BMMSCs — meaning the stem cells had been grown in the media, allowing them to release their signaling molecules, and then the stem cells were removed so that only those signaling molecules remained. (Media refers to the solution carrying the nutrients necessary for cells to grow.)
In a mouse model of Sjögren’s syndrome, treatment with DPSC-conditioned media (injected into the bloodstream twice per week) significantly increased salivary flow and decreased markers of inflammation, whereas BMMSC-conditioned media had little effect.
“These results suggest that DPSC-[conditioned media] injection was effective in alleviating the decrease in fluid secretion and maintaining normal secretory function,” the researchers wrote.
Further investigation in the mouse model suggested that treatment with DPSC-conditioned media promoted the development of regulatory T-cells (Tregs). These cells act like the “brakes” of the immune system, sending cellular signals to decrease inflammation and promote wound healing. Of note, in Sjögren’s syndrome, Treg levels are typically decreased.
In contrast, treatment with DPSC-conditioned media decreased levels of pro-inflammatory T-cells (specifically Th1 and Th17 cells) and antibody-producing cells, which are typically present at higher-than-normal levels in Sjögren’s and help to drive damaging inflammation.
Treatment with DPSC-conditioned media also reduced apoptosis (a type of cell death) in the mice’s salivary glands.
“This study reveals a new effect of DPSC-[conditioned media] and provides a therapeutic strategy for [Sjögren’s syndrome],” the researchers concluded.