Study Links Altered Gut Microbiome in Sjogren’s to Systemic Inflammation
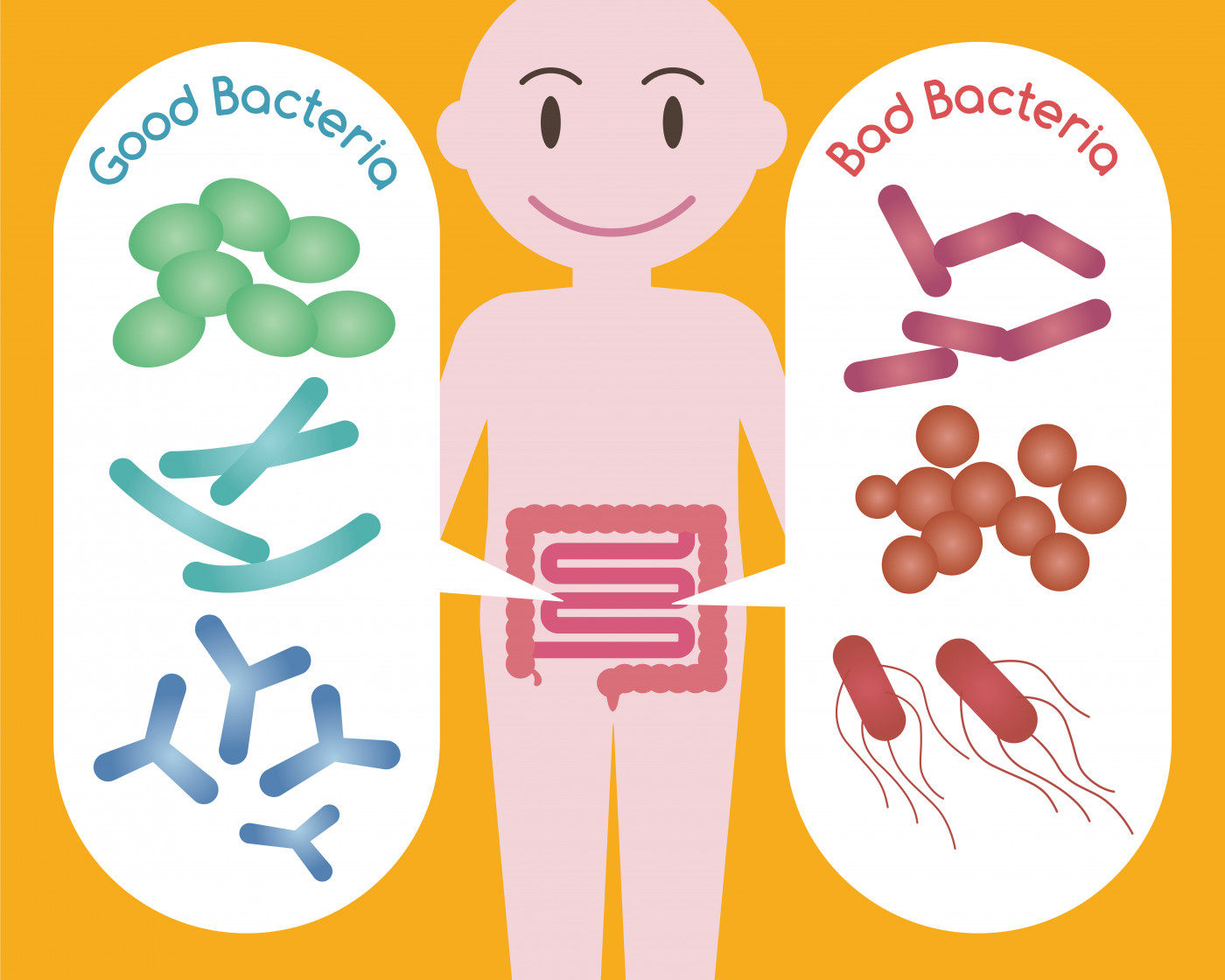
Primary Sjogren’s syndrome (pSS) patients have less diversity in their gut microbiome — with less abundant beneficial bacteria but more abundant opportunistic bacteria with pro-inflammatory activity — compared with healthy people, a study suggests.
Patients also had higher levels of pro-inflammatory immune signaling molecules, which were associated with the presence of disease-causing bacteria in the gut.
These findings suggest a role for the gut microbiome in Sjogren’s syndrome and may help in the development of therapies that control microbiome-driven inflammation.
The study, “Connection between the Gut Microbiome, Systemic Inflammation, Gut Permeability and FOXP3 Expression in Patients with Primary Sjögren’s Syndrome,” was published in the International Journal of Molecular Sciences.
Sjogren’s syndrome is an autoimmune inflammatory disorder primarily characterized by chronic inflammation of the salivary and lacrimal (tear) glands, but that can also affect other tissues, including the brain, lungs, and gastrointestinal tract.
Recent studies have reported differences in microbes in the gut and oral cavity of Sjogren’s patients compared with controls. Given the interplay between the gut microbiome, the cells that line the gut surface (epithelium), and immune cells, these changes may affect local and systemic inflammation, impacting disease.
In the new study, researchers based at the University of Córdoba, in collaboration with colleagues at the Biomedical Research Institute of Malaga in Spain, analyzed the gut microbiome of people with primary Sjogren’s syndrome and related these findings to inflammation.
The study included 19 women with Sjogren’s (mean age of 56.4 years) plus 19 age-matched healthy women as controls. Bacteria were identified by DNA analysis of stool samples, while blood samples were collected to test for various molecules associated with inflammation.
In patients, the diversity and richness of gut microbes within individual samples (alpha diversity) was decreased compared to controls, and the diversity between samples (beta diversity) showed patients had microbe populations that were distinct from controls, “indicating significant disease-mediated microbial changes,” the researchers wrote.
Significant differences in microbe types were found between patients and controls. Patients had an increased abundance of bacteria associated with disease, including Clostridium, Enterobacter, Escherichia, and Streptococcus, as well as Prevotella, a group of bacteria linked to the onset of the autoimmune condition rheumatoid arthritis.
Compared to controls, patients had a decreased abundance of bacterial groups such as Parabacteroides, Faecalibacterium, Roseburia, Ruminococcus, Dorea, Alistipes, and Blautia. Also depleted were Bacteroides, which have been shown to balance anti-inflammatory and pro-inflammatory immune cells, and Bifidobacterium, which are reduced in people with rheumatoid arthritis and the intestinal inflammatory condition Crohn’s disease.
The microbes in individuals with Sjogren’s were enriched with genes from biological pathways associated with bacterial infection causing disease and chronic inflammation.
In patients, blood tests revealed significantly higher levels of the protein zonulin, which modulates the permeability of cells of the digestive tract wall, suggesting more intestinal permeability in those with Sjogren’s.
Also, patients had significantly higher levels of pro-inflammatory immune signaling proteins (cytokines), including interleukin (IL)-6, IL-17, IL-12, and TNF-alpha, and significantly lower concentrations of the anti-inflammatory cytokine IL-10.
Compared to controls, patients had significantly lower production of a protein expressed in immune cells called FOXP3, essential for the normal of regulatory T-cells, which play an important role in preventing autoimmunity.
Statistical analysis showed that higher zonulin levels were associated with a higher abundance of the bacteria Prevotella copri, which produce enzymes capable of degrading mucus on the intestinal surface.
Higher levels of zonulin (increasing gut permeability) and Prevotella microbes may allow disease-related molecules to enter tissues and the bloodstream, “resulting in the immune activation and tissue inflammation important in the onset or progression of several intestinal and chronic autoimmune diseases,” the investigators wrote.
Higher levels of zonulin, as well as pro-inflammatory cytokines IL-17, IL-12, and TNF-alpha, were associated with a lower abundance of rheumatoid arthritis-related bacteria Bifidobacterium in patients.
More IL-12 was also associated with the increased abundance of Enterobacter, and higher IL-6 levels were linked with higher numbers of Escherichia coli, both disease-causing bacteria.
The significant increase in these two bacteria, and the correlations found between gut microbes and levels of cytokines and FOXP3 production, suggested that the depletion of bacteria with anti-inflammatory properties and those that improve gut barrier function “could increase intestinal permeability and low-grade inflammation in pSS patients,” the researchers wrote.
“Further studies are needed to better understand the real impact of [gut bacteria imbalance] on the course of pSS and to conceive preventive or therapeutic strategies to counteract microbiome-driven inflammation,” they concluded.