Primary Sjögren’s Syndrome May Rarely Manifest as a Stroke, Case Report Shows
Written by |
Physicians in Cincinnati have reported the rare case of a woman whose first symptom of primary Sjögren’s syndrome was intracranial bleeding.
While rare — only two similar cases have been described to date — increasing awareness about the neurological manifestations of the disease could lead to prompt treatment of these patients, improving their prognosis.
The study, “A rare case of Sjögren’s Syndrome associated with Intracranial Hemorrhage- case report and literature review,” was published in the International Journal of Clinical Rheumatology.
Sjögren’s syndrome is an autoimmune disease characterized by abnormal infiltration and accumulation of immune cells inside some glands, leading to inflamed tissues. Eventually, the damage is irreparable.
Problems in the peripheral nervous system are common in Sjögren’s syndrome patients, but those affecting the central nervous system are extremely rare. Since 1982, only 15 cases of stroke have been described in primary Sjögren’s syndrome patients, and only two of those involved with intracranial bleeding.
In this case, researchers reported that a 61-year-old Ohio woman who experienced an intracranial hemorrhage, or bleeding, was her first manifestation of Sjögren’s syndrome.
The woman arrived at the emergency room, complaining of worsening headaches, dizziness, nausea, vomiting, and extreme sensitivity to light.
She had a medical history of Hashimoto thyroiditis — an autoimmune condition in which the immune system attacks the thyroid — and cervical cancer, osteoarthritis, and migraines. She had been receiving treatment for migraines for the past year.
When she was admitted, the patient was confused and lethargic, but a neurological examination showed a normal response to stimulus, normal reflexes, and full strength in all extremities. This suggested no problems in the peripheral nervous system.
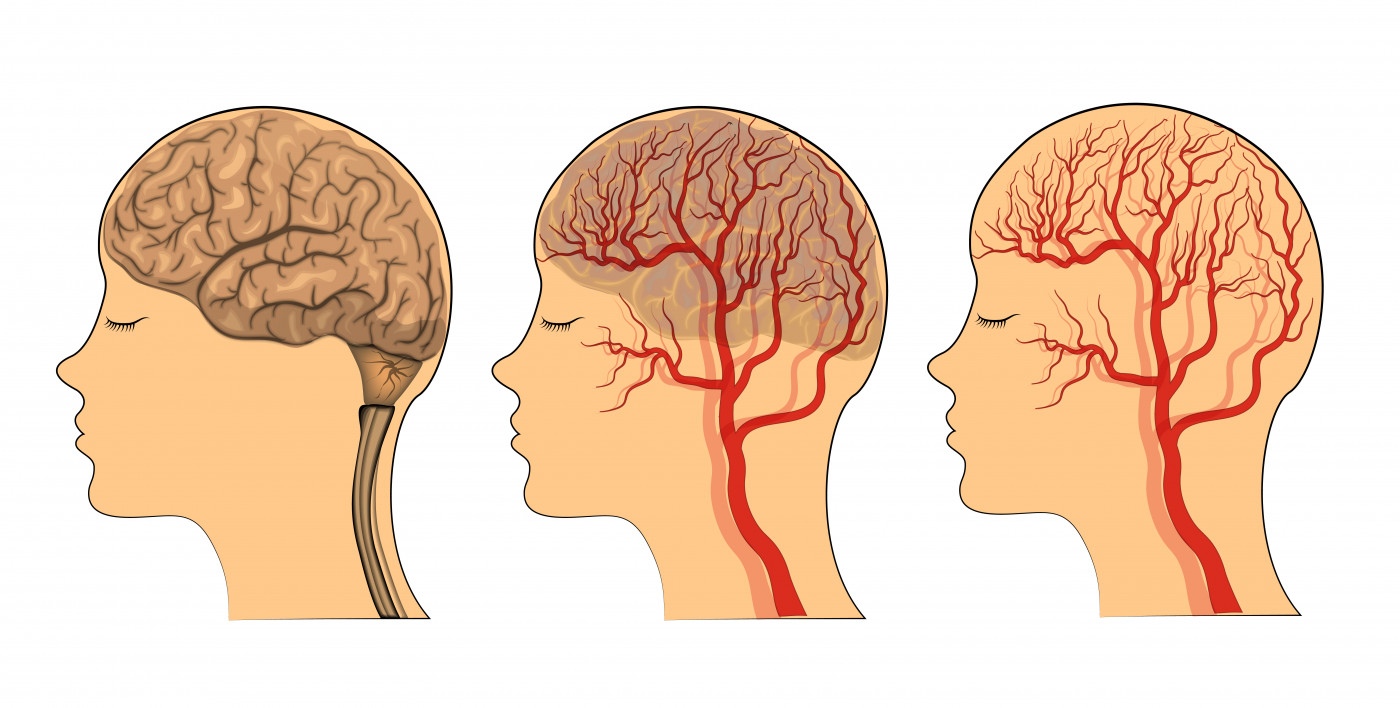
An electroencephalogram (EEG) also retrieved negative results for acute seizures. However, a computed tomography of the head revealed signs of stroke, which was causing her to bleed into the space surrounding the brain (a subarachnoid hemorrhage, or SAH).
Magnetic resonance imaging confirmed the SAH diagnosis, and the patient received surgery to remove the bleeding. However, she lacked blood clots that could explain the hemorrhage, leading the team to investigate the woman’s clinical history in detail.
They found that a long history of eye dryness, mouth dryness, and occasionally swelling of the parotid gland (a major salivary gland), along with multiple tooth decays, cavities, and bad breath.
Over the past 2-3 months, the patient also had lost nearly 20 pounds unintentionally, had decreased appetite, night sweats, jaw and axilla pain, and also experienced short term memory loss.
Blood examination confirmed the presence of Sjögren’s-related autoantibodies in circulation, and a biopsy to her salivary glands showed infiltration of immune cells, leading to a final diagnosis of Sjögren’s syndrome.
After receiving high-dose intravenous methylprednisolone for three days, followed by daily prednisone, the patient’s mental status improved significantly, and she was discharged to acute rehabilitation.
One month later, blood exams came back normal, with no signs of inflammation.
“Stroke is an extremely rare manifestation of primary Sjögren’s syndrome,” the researchers wrote. “Our case emphasizes the importance of a taking a detailed history in intracranial hemorrhage cases,” which may help detect an autoimmune origin.
“Increasing awareness about the neurologic manifestations of [Sjögren’s syndrome] may lead to prompt treatment and better prognosis of these patients,” investigators concluded.





