Primary Sjögren’s ‘Clusters’ Could Improve Treatment Precision
Written by |
A new method for dividing people with primary Sjögren’s syndrome (pSS) into subgroups based on detailed molecular differences may help improve precision treatment for patients, a recent study suggests.
The findings “have major implications for the treatment of pSS patients,” researchers wrote, as they could help unravel the causes of the disease and identify likely targets for treatment in specific patients.
The study, “A new molecular classification to drive precision treatment strategies in primary Sjögren’s syndrome,” was published in Nature Communications.
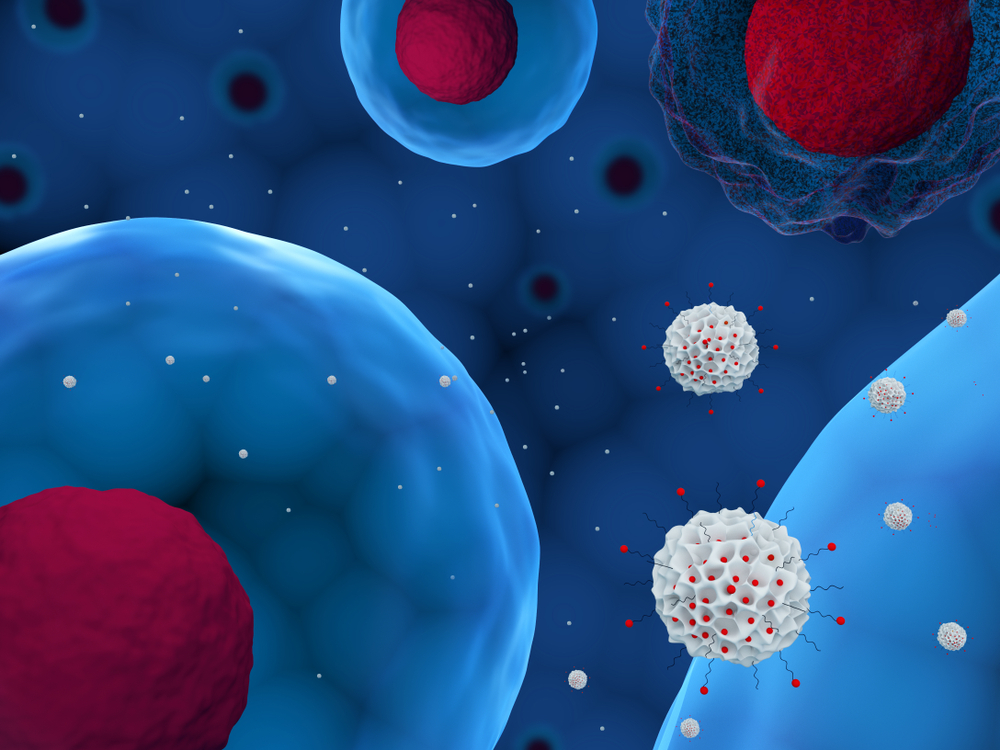
Primary Sjögren’s syndrome is caused by the immune system erroneously attacking the body’s healthy tissues. The tear and salivary glands are mainly affected in primary Sjögren’s syndrome, but other bodily systems also may become involved.
One of the obstacles in designing effective treatments for Sjögren’s syndrome is that symptoms vary from person to person — and there likely are variations in the underlying biology that drives the disease, which is still incompletely understood.
In the new study, an international team led by researchers in France performed extremely detailed biological analyses in order to better understand the differences among Sjögren’s patients. Collectively, the team analyzed data for 304 primary Sjögren’s syndrome patients, as well as 330 healthy volunteers, matched in terms of age and sex, for comparison.
The team first looked at transcriptomic data — looking at which genes are “turned on” or “turned off” — in blood samples. These data were fed into computer algorithms, which divided the patients into four groups, or clusters, discriminated by differences in 257 genes.
The researchers further characterized the clusters with a battery of other biological and genetic assessments, including looking at specific types of immune cells and immune signaling molecules in the blood, assessing mutation patterns, and looking at changes in epigenetics (how DNA is “packaged” in cells, which affects how genes are “read”).
Each cluster had specific molecular features. For example, the transcriptomic, mutation, and blood cell profiles in Cluster 2 were most similar to those in healthy volunteers. Cluster 2 also had a higher proportion of patients treated with anti-malarial medications, and a shorter disease duration, compared to the other clusters.
By contrast, relative to the healthy samples, Clusters 1, 3, and 4 all were characterized by abnormally high interferon activity. Interferon, or IFN, encompasses a set of signaling molecules that drive inflammation in many autoimmune diseases. The specific types of IFN responses (each characterized by different sets of specific molecules) varied among these three clusters, though the Type I IFN response was elevated in all three.
Also of note, the frequency of B-cells — a type of immune cell that makes antibodies, among other functions — was increased substantially in Cluster 3, relative to the other clusters.
The study findings may have implications for treatment. “Our findings provide a strong rationale for treating patients with either a C1, C3, or C4 profile with inhibitors of type I IFN responses alone or in combination as they support the relevance of B cells as potential therapeutic targets in C3 patients,” the researchers wrote.
Using machine learning, the team developed a model that allowed patients to be grouped into each of the four clusters based on the expression (production) of just a few dozen genes. The model was more than 95% accurate, analyses showed.
The researchers proposed that using this model to classify patients could help to personalize treatment, and allow greater precision when enrolling participants in clinical trials for investigational treatments. The team noted that such approaches already have shown promise in certain cancers.
“Our results can improve pSS treatment strategies allowing a patient centric approach. This paradigm already implemented in the oncology field will increase the probability of trial successes and boost the development of new efficient drugs against pSS,” the researchers concluded.