Immune T-Cells May Be Useful Indicator of Disease Activity
Written by |
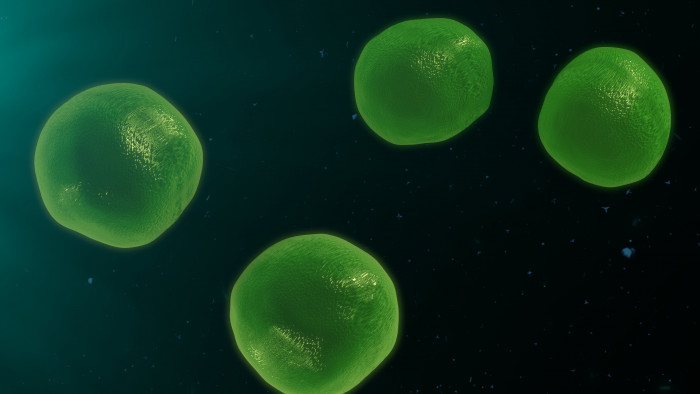
Immune T-cells
A subset of immune cells, called CD4+CD8+ T-cells, is increased in the blood of patients with Sjögren’s syndrome, and their levels seem to correlate with lower disease activity, according to a small study.
The findings suggest doctors could make use of those cells to track or even control how the disease is progressing.
The study, “Increased CD4+CD8+ Double-Positive T Cell in Patients with Primary Sjögren’s Syndrome Correlated with Disease Activity,” was published in the Journal of Immunology Research.
Over the past few years, researchers have started to recognize that a subset of immune T-cells called CD4+CD8+ T-cells may play an important role in autoimmune diseases. In Sjögren’s syndrome, however, their role remains unknown.
Researchers in China set out to determine the amount of these cells circulating in the blood of Sjögren’s patients and how it correlates with disease activity. Their ultimate goal was to understand the significance of CD4+CD8+ T-cells in disease progression.
The study enrolled 35 patients with primary Sjögren’s syndrome and 35 healthy controls who were matched for age and sex. Participants had been admitted to the Nanjing Drum Tower Hospital from January to June 2019.
First, the researchers counted the number of CD4+CD8+ T-cells in circulation. Using a technique called flow cytometry, which allows researchers to count the number of cells displaying certain proteins on their surface, they found that the median proportion of CD4+CD8+ T-cells was significantly higher in people with Sjögren’s syndrome than in controls.
Of the 35 patients with Sjögren’s syndrome, 16 had received immunosuppressants — a type of medication that suppresses the immune system — prior to admission. The proportion of CD4+CD8+ T-cells was similar between those who had received immunosuppressants and those who had not.
To address if the increased proportion of CD4+CD8+ T-cells could have any clinical significance, the team then investigated whether levels of these cells correlated with any demographic or clinical parameters.
The proportion of CD4+CD8+ T-cells did not increase with age. However, it correlated negatively with erythrocyte sedimentation rate — a blood parameter that helps detect inflammation.
It also correlated negatively with two of the most common types of immunoglobulins, known as IgA and IgG. Immunoglobulins, also known as antibodies, are often increased in patients with Sjögren’s disease, as a reflection of an overactive immune system.
One way T-cells work is via the release of cytokines — chemical signals that are key in immune response. One such cytokine, called interleukin 10 (IL-10), is a known anti-inflammatory factor that protects against autoimmunity.
In the study, a number of cytokines, both anti- and pro-inflammatory, were found to be increased in Sjögren’s patients. However, only IL-10 levels were significantly associated with a greater proportion of CD4+CD8+ T-cells, suggesting that these cells are producing the anti-inflammatory molecule.
In line with this, patients with a higher proportion of CD4+CD8+ T-cells had less disease activity, as measured with the EULAR Sjögren’s disease activity index and the Sjogren’s syndrome disease activity index.
The findings suggested CD4+CD8+ T-cells “may play a protective role in the pathogenesis [how a disease develops] and progression” of Sjögren’s syndrome, the researchers wrote.
Because the proportion of these cells appeared to be tied to the clinical manifestations of Sjögren’s syndrome, it may be used “as an indicator for disease activity.” On the other hand, this immune cell subtype may also be a potential “new strategy for treatment,” the researchers added.