Hydroxychloroquine Lowers Cardiovascular Risk in Sjögren’s Patients, Study Suggests
Written by |
Long-term use of hydroxychloroquine significantly lowers the risk of coronary artery disease, the most common form of heart disease, in people with Sjögren’s syndrome, a data study in Taiwan suggested.
Its cardiovascular protective effects, in addition to a wider range of benefits, suggest the medication may control the clinical manifestations of Sjögren’s, the researchers wrote.
The study, “Cardiovascular Protection of Hydroxychloroquine in Patients with Sjögren’s Syndrome,” was published in the Journal of Clinical Medicine.
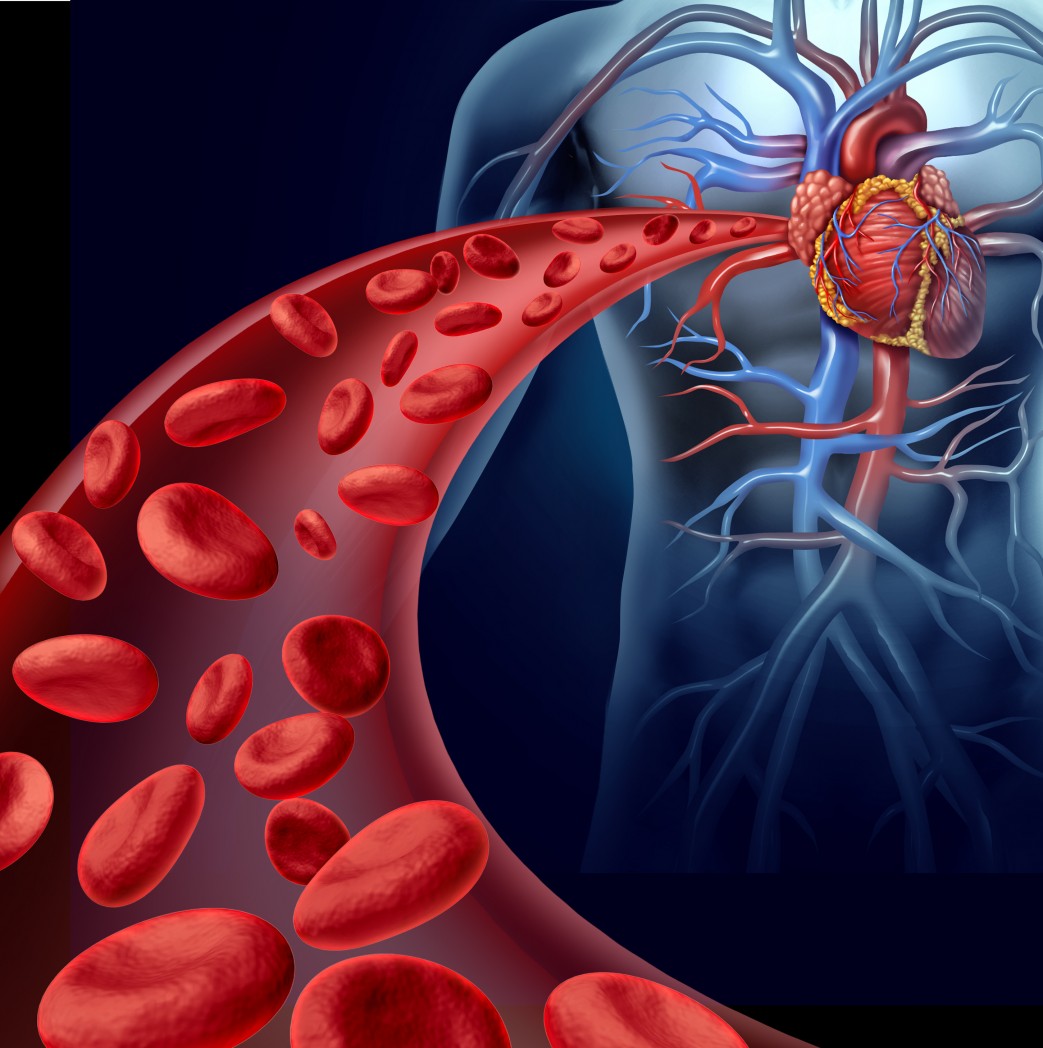
Sjögren’s patients have a higher than usual incidence of coronary artery disease (CAD), which is characterized by the narrowing or blockage of the coronary arteries that supply blood to heart muscle.
CAD is usually caused by a buildup of fatty deposits in arteries and an increased arterial stiffness, which are also more common in people with Sjögren’s.
Hydroxychloroquine, an anti-malarial, has been widely used to treat autoimmune conditions like lupus, rheumatoid arthritis, and Sjögren’s. It works to modulate the immune system, which is overly active in these disorders, and also seems to reduce lipid levels and protect against blood clots and diabetes.
Evidence suggests that hydroxychloroquine protects against cardiovascular disease in people with autoimmune diseases, but whether this medication can lower the risk of CAD in Sjögren’s patients remains unclear.
Researchers in Taiwan investigated data covering 1,142 newly diagnosed Sjögren’s patients included in the country’s National Health Insurance Research Database (NHIRD). Participants were age 20 or older, had been diagnosed from 2000–12, and started treatment with hydroxychloroquine within one year of their diagnosis. All were followed through December 2013 unless they developed CAD or left this insurance program.
To determine adherence to hydroxychloroquine use, each patient was assigned a medication possession ratio (MPR) — a way of estimating treatment adherence. MPR is the proportion of days since treatment initiation in which a patient actually uses the medication. An MPR close to one indicates high adherence to treatment; numbers closer to zero indicate poor adherence.
Based on their MPR scores, participants were divided into three groups: those with a low adherence (MPR scores below 0.40), an intermediate adherence group (MPR between 0.40 and 0.69), and a high adherence group (MPR scores of 0.70 or greater).
Patients in each group were fairly similar in terms of incidences of high blood pressure, diabetes, chronic obstructive pulmonary disease, or stroke. But the high adherence group had a smaller proportion of patients with high lipid (fat) levels — a risk factor for CAD — compared with the low adherence group (3.3% vs. 7.8%).
Consistent with those findings, patients in the high compliance group were about 50% less likely to develop CAD than those with poor adherence to hydroxychloroquine, a significant difference.
Study findings also confirmed several other CAD risk factors, including older age, high blood pressure, and high lipid levels. Regardless of medication compliance, Sjögren’s patients who also had chronic obstructive pulmonary disease were 3.6 times more likely to develop CAD than those without this comorbidity (concurrent disease).
Since age is a risk factor for CAD, the researchers examined the effects of hydroxychloroquine adherence across age groups. While treatment use did not affect CAD incidence in younger and older patients, those ages 40 to 64 had a significantly lower risk of CAD with high adherence to treatment. These patients were 72% less likely to have CAD than those of the same age group who were poor compliers.
Interestingly, this finding appeared to be sex-specific. Women in the 40–64 age group who were highly compliant had a lower risk of CAD that did those at these ages who were poorly compliant — a difference was not observed in male groups of similar ages. But, this absence “may be due to the small number of males in our study,” the researchers wrote.
“HCQ [hydroxychloroquine] may be used to control the clinical manifestations of SS [Sjögren’s syndrome],” the researchers wrote.
“Significant cardiovascular protection of long-term HCQ therapy was observed from our findings. Therefore, adequate immunotherapy of HCQ is suggested in the patients with SS,” they concluded.