Early Sjögren’s treatment improves recovery from stroke: Study
Prompt care also found to reduce recurrence for primary Sjögren’s patients
Written by |
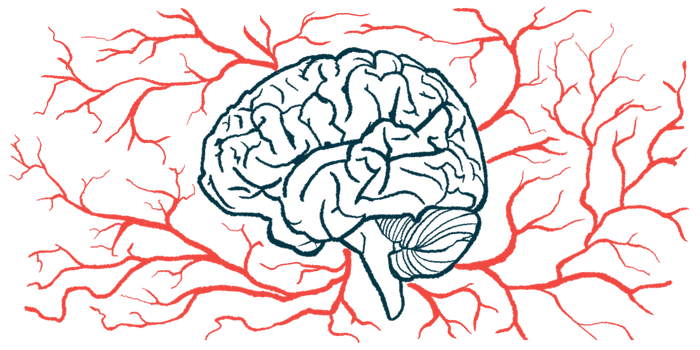
Prompt treatment for primary Sjögren’s disease in patients who develop ischemic stroke, where parts of the brain die due to the lack of blood flow, helps to promote neurological recovery and reduce the risk of stroke recurrence, a single-center study in China found.
In fact, the researchers reported that “the recurrence rate of [ischemic stroke] was 0% in the treatment group but 33.3% in the nontreatment group” among patients, based on whether they had been treated for primary Sjögren’s.
“This study emphasizes the importance of pSS [primary Sjögren’s disease] as a high-risk factor [for ischemic stroke] and the necessity of pSS-related screening for [ischemic stroke] patients,” the researchers wrote.
According to the researchers, “our study found that timely and effective intervention treatment of pSS can improve the prognosis of patients.”
Titled “Primary sjögren’s syndrome among patients with cerebral infarction,” the study was published in the journal Scientific Reports.
Sjögren’s disease is an autoimmune condition primarily characterized by inflammation of the glands that produce tears and saliva. Its hallmark symptoms are eye and mouth dryness. Patients often test positive for self-reactive antibodies, such as anti-Ro (or SSA) and anti-La (or SSB) antibodies.
The disease can be classified as primary if it appears on its own, or secondary when it’s associated with another condition.
Increased risk of stroke reported for primary Sjögren’s patients
In some patients, primary Sjögren’s also affects the central nervous system (CNS), comprised of the brain and spinal cord — sometimes even before the typical glandular manifestations. Some studies have reported an increased risk for cerebrovascular diseases, including ischemic stroke, also called cerebral infarction, in this patient population.
“However, because both patients and clinicians have always ignored symptoms such as the dry mouth and dry eyes, it is not always possible to diagnose pSS before patients are admitted to the hospital for [cerebrovascular disease],” the researchers wrote.
The team also noted that some people experiencing ischemic stroke have high recurrence rates, despite traditional control of risk factors and active preventive treatment.
“We found that these patients often have pSS and they have not been actively intervened or treated regularly,” the team wrote.
Now, to gain a better understanding of the clinical features, treatment, and outcomes of this group of patients, the researchers retrospectively analyzed data from 27 people with ischemic stroke and primary Sjögren’s. All were followed up for more than one year.
The patients were divided into two groups based on whether they received immunomodulatory medications for primary Sjögren’s (12 individuals) or not (the remaining 15) after the ischemic stroke. These medications included the corticosteroid methylprednisolone and hydroxychloroquine.
Because both patients and clinicians have always ignored symptoms such as the dry mouth and dry eyes, it is not always possible to diagnose [primary Sjögren’s disease (pSS)] before patients are admitted to the hospital for [cerebrovascular disease, including ischemic stroke]. … These patients often have pSS and they have not been … treated regularly.
The average age of the patients was similar between the groups (59.1 vs. 55.8 years). In the treatment group, two-thirds of the patients were women. The group not receiving treatment was nearly evenly split by sex.
Most patients had eye or mouth symptoms before the ischemic stroke (66.7% vs. 73.3%). There also was a similar prevalence of risk factors for cerebrovascular disease, such as smoking, drinking, high blood pressure, diabetes, and elevated levels of the fatty molecule cholesterol.
The most common clinical manifestations included limb numbness and weakness (48.1%), dizziness and headache (25.9%), and vague speech (22.2%).
Except for one patient, all were diagnosed with primary Sjögren’s during hospitalization for ischemic stroke. The diagnoses were based on tear production, salivary gland biopsy, saliva production, and the presence of anti-SSA/anti-SSB antibodies.
Brain MRI findings revealed that most patients had small blood vessel lesions with multiple sites of tissue death in deeper brain regions, but no large areas of damage.
Favorable prognosis twice as likely for treated patients after 1 year
After one year of treatment, the rate of favorable prognosis was twice as high in the treatment group compared with the nontreatment group (83.3% vs. 40%). Favorable prognosis was reflected by a score below two in the modified Rankin Scale (mRS), which assesses disability and dependence in daily activities, and where higher scores indicate worse disability.
In addition, recurrence of ischemic stroke occurred in one-third of the nontreated patients, but none of those given treatment.
Further statistical analyses showed that treated participants were 7.5 times more likely to have a favorable prognosis, and 89% less likely to experience another event relative to those not given treatment.
The researchers noted that their findings can provide key guidance to clinicians.
“For the [ischemic stroke] patients, clinicians should carefully investigate whether they have [eye] and oral symptoms,” the team wrote. “And if they have, and are accompanied by anti-SSA/anti-SSB positivity, it is necessary to further [test saliva and tear production] to confirm the diagnosis.”
The researchers noted that, “when pSS has been identified in [ischemic stroke] patients, prompt immunomodulatory therapies for pSS will facilitate neurofunctional recovery and reduce [stroke] recurrence,” the team concluded.