Arthritis Medicine Tocilizumab Treats COVID-19 in Elderly Patient
Written by |
Tocilizumab, a medicine approved for certain types of arthritis, may be a safe and effective approach for treating severe respiratory distress associated with COVID-19 in people with autoimmune conditions, the case of an elderly Sjögren’s syndrome patient suggests.
The report, “Immediate Amelioration of Severe Respiratory Distress in Sjögren’s Syndrome with COVID-19 Treated with a Single Dose of Off-label Tocilizumab,” was published in the journal Internal Medicine.
Sjögren’s syndrome and other rheumatic disease have not been directly associated with an increased risk for COVID-19. But the use of medications that suppress the immune system puts these patients at a greater risk of severe disease requiring hospitalization should they contract COVID-19.
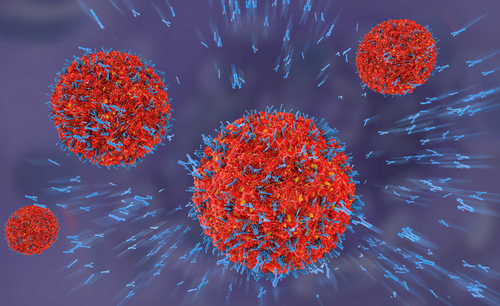
In some patients with COVID-19, it is not the virus itself that does the worst damage. Instead, this virus triggers excessive production of immune cells and their inflammatory molecules in a life-threatening reaction known as cytokine storm, which causes severe lung damage and acute respiratory distress.
Interleukin (IL-6) signaling is the main culprit of this uncontrolled immune reaction in COVID-19 patients. Thus, it has been suggested that IL-6 inhibitors, such as tocilizumab (sold as Actemra by Genentech), may effectively control lung damage induced by the virus.
Now, researchers at the Sapporo City General Hospital, in Japan, described the case of an 85-year-old man with Sjögren’s syndrome who developed severe shortness of breath and respiratory distress related to COVID-19.
“The patient had risk factors for the rapid deterioration of COVID-19, including an older age … corticosteroid use, and hypertension,” they wrote. However, he was successfully treated with tocilizumab.
Prior to his COVID-19 diagnosis, the patient was being treated with low-dose methylprednisolone for salivary gland swelling and joint inflammation related to Sjögren’s syndrome. He initially visited his physician with a fever and cough.
After a chest X-ray and CT scan came back normal, the patient was prescribed antibiotics for five days. But his symptoms worsened and he began experiencing progressive shortness of breath. A second X-ray and CT scan revealed opacities in both lungs, and a positive COVID-19 test confirmed the diagnosis.
Following his discharged from the hospital, the patient began experiencing a sustained fever, loss of appetite, and low urine output. Eleven days after his initial symptoms, the man was admitted to the emergency room with low oxygen levels, an elevated respiratory rate, and fever.
Blood test results revealed elevated levels of iron, D-dimer, and IL-6, which were suggestive of severe COVID-19 critically complicated by respiratory distress.
The second week of COVID-19 onset is sometimes characterized by the worsening of existing symptoms, as well as the emergence of new ones. The cause of this “second wave” is unknown, but it’s thought to result at least in part from a cytokine storm.
Thus, the patient received a single 480 mg intravenous (into-the-vein) dose of off-label tocilizumab — meaning it was prescribed for a use other than that for which it was approved — to lower the levels of inflammatory molecules. He also was given a short-term increase of prednisolone to 20 mg/day to prevent the worsening of Sjögren’s symptoms.
The man’s symptoms rapidly improved, allowing prednisolone tapering and the discontinuation of oxygenation. He was discharged after 21 days of hospitalization.
Of note, this medication is approved for treating a form of cytokine storm that occurs after treatment with some immunotherapies. Tocilizumab has shown promise as an off-label treatment for the management of COVID-19 patients, but less evidence exists regarding tocilizumab’s use in people with autoimmune conditions.
“Therefore, this is an elderly case showing additional evidence supporting the promising effect of IL-6 inhibition on severe COVID-19 in patients with autoimmune diseases,” the researchers concluded.