Patients with Primary Sjogren’s Syndrome Can Develop Inflammation of Large Blood Vessels
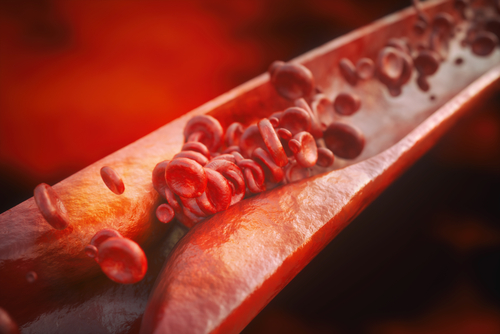
While rare, patients with primary Sjogren’s syndrome can develop central nervous system disease due to involvement of large blood vessels, rather than small or medium-sized blood vessels, according to a new case study.
The study, “Cerebral Large-Vessel Vasculitis in Sjogren’s Syndrome: Utility of High-Resolution Magnetic Resonance Vessel Wall Imaging,” was published in the Journal of Clinical Neurology.
Patients with Sjogren’s syndrome, an autoimmune disease, mostly experience dryness of the mouth and eyes as result of inflammation in the glands producing these secretions.
Sometimes, patients with Sjogren’s syndrome also exhibit involvement of the central nervous system (CNS). They can develop a multiple sclerosis-like presentation with lesions in brain, cranial nerve palsies (lack of nerve function), and myelitis (inflammation of the spinal cord).
Inflammation of small blood vessels often has been hypothesized as a potential mechanism that underlies CNS involvement in Sjogren’s syndrome. The involvement of larger blood vessels in Sjogren’s syndrome has been reported only rarely.
Now, researchers at the Sree Chitra Tirunal Institute for Medical Sciences and Technology in India reported the case of a 50-year-old woman who developed inflammation in large brain vessels secondary to Sjogren’s syndrome.
The patient presented with recurrent episodes of transient ischemic attacks — a brief episode of neurological dysfunction caused by loss of blood flow to the brain, spinal cord, or retina.
She experienced complete recovery of symptoms after several minutes, and also had two episodes of minor stroke with recovery after two days.
The patient had dryness of the eyes. Hence, physicians conducted laboratory testing and found that routine blood parameters, cerebrospinal fluid study, and inflammation markers were normal.
Interestingly, the antibody profile revealed strong positivity for two Sjogren’s antibodies — anti-SSA/Ro and anti-SSB/La. Additionally, Schirmer’s test was positive for dry-eye syndrome. So, results suggested that the patient had Sjogren’s syndrome.
Upon conducting a head CT scan, physicians discovered infarcts — a small localized area of dead tissue resulting from failure of blood supply — in the cerebral arteries (large blood vessels of the cerebrum). The cerebrum (the largest part of the human brain) is responsible for voluntary functions and higher order brain function, such as thought and action.
CT angiography, which measures narrowing of a blood vessel, also revealed that certain cerebral blood vessels were narrower.
Then, a special kind of magnetic resonance imaging that examines blood vessels revealed wall thickening of the large right internal carotid artery (ICA) without any significant remodeling of the artery, which suggested that the patient had vasculitis of the terminal right ICA and its branches.
The physician diagnosed the patient with large-vessel vasculitis secondary to Sjogren’s syndrome.
The patient was treated with intravenous methylprednisolone (a corticosteroid which reduces inflammation) for five days, followed by oral prednisolone (another corticosteroid), along with mycophenolate mofetil (an immunosuppressant) and hydroxychloroquine (an anti-inflammatory).
At the three-month follow-up, the patient did not experience any further events related to restriction in brain blood supply.
“This case demonstrates vasculitis of cerebral large-vessels in a patient with primary Sjogren’s syndrome and provides further insight into the pathogenesis of the CNS involvement in Sjogren’s syndrome,” investigators wrote.
“Our patient had dry-eye syndrome, based on a positive Schirmer’s test, and strong positivity for SSA/Ro and SSB/La, suggestive of Sjogren’s syndrome. The presence of right supraclinoid ICA [narrowing] in a setting of primary Sjogren’s syndrome suggested a vasculitic etiology,” they added.
Interestingly, while vasculitis involving small and medium-size vessels have been demonstrated in patients with Sjogren’s syndrome, large vessel involvement in Sjogren’s syndrome is rare, with only three cases reported in the literature.
“Our case highlights the presence of vasculitic involvement of the large cerebral vessels in primary Sjogren’s syndrome, which can be confirmed by [magnetic resonance imaging],” they concluded.






